Remember when we were all anxiously looking forward to the end of 2020 and anticipating 2021? It’s hard to believe 2021 is now almost over. Healthcare continues to move at such a fast pace, making it especially worthwhile to take stock of your organization’s greatest challenges heading into 2022.
We recently asked healthcare leaders to get more specific about their greatest challenges. The results are in:
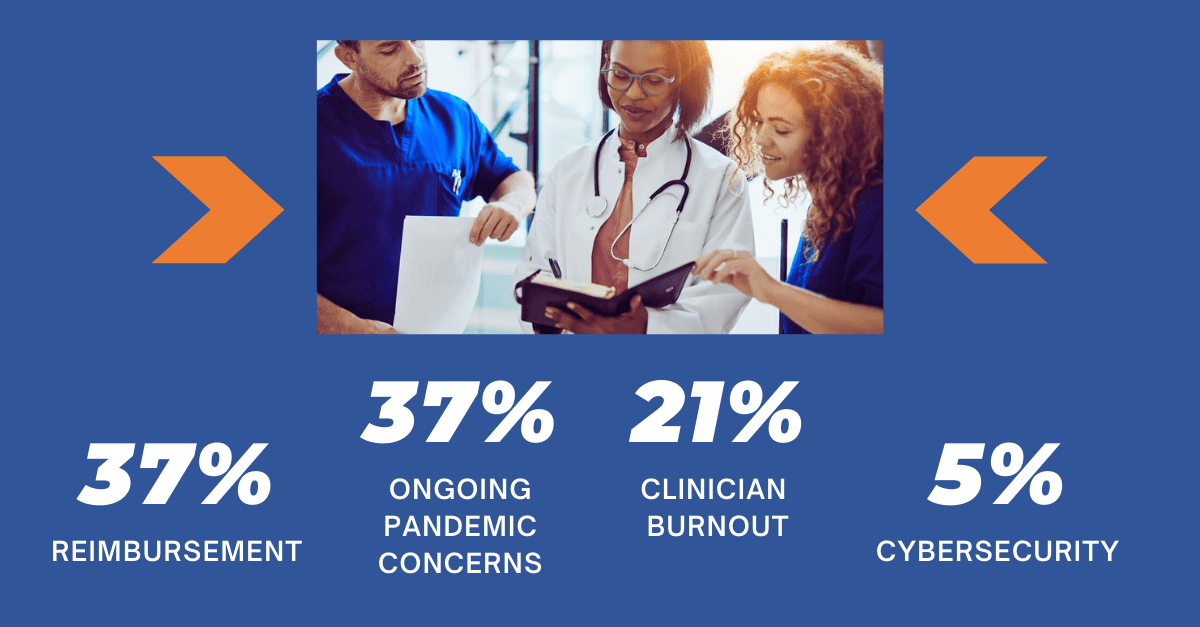
Let’s take a closer look into these 4 concerns and their impact on the upcoming new year.
Reimbursement
Many healthcare systems have recently faced historically low revenues. Some faced cancellations or postponements of outpatient and elective surgeries, and some faced a fluctuating challenge of caring for those without health insurance.
CMS released its proposed physician payment rule for 2022, and it includes a host of changes. One such change – and an area of concern – is a reduction in the physician fee schedule.
Todd Askew, the AMA’s senior vice president of advocacy, noted physicians are still impacted by the volume reduction caused by the pandemic and that the “across the board 3.75% cut is going to hurt.” He also noted the cut is not sustainable and the AMA is working to convince Congress to “further delay or cancel some of these or all of these payment decreases that could impact physicians in the coming year.”
The full impact certainly remains to be seen, but a flurry of calculations heading into 2022 is to be expected.
For more on recent reimbursement challenges that may shape your organization’s approach to 2022, click here.
Ongoing pandemic concerns
The keyword here is ongoing. The healthcare system continues to naturally evolve, but there is no doubt that those working inside this complex community are exhausted from the pandemic. It’s anyone’s guess what the pandemic may look like in 2022, but there are some promising predictions out there:
- From vaccine makers: There could be an end to the pandemic in 2022 and the coronavirus may likely become similar to the common cold.
- From the Centers for Disease Control and Prevention: “The delta surge appears to be peaking nationally, and cases and deaths will likely decline steadily now through the spring without a significant winter surge.”
However, other research shows the next few months will see hospitals continue to struggle:
- From Bloomberg: There will likely be more surges and a possible vaccine-resistant variant. To be sure, healthcare is weary, yet bracing for more. This means that struggles related to staffing, supply chain, capacity, and resource allocation continue.
- From IHME: “Hospital systems, however, in the Northern Hemisphere may be under just as severe stress because of the combined impact of flu – which we expect will be considerable this year – along with moderate levels of demand for hospitalization and ICU beds for COVID. Unfortunately, health care workers and health care systems in the Northern Hemisphere may not see a winter that is better than last year.”

For more on healthcare workplace lessons from the pandemic, click here.
Clinician burnout
In an NPR article last week, New York City ICU nurse Matthew Crecelius characterized clinician burnout as “like watching a bomb go off in slow motion,” and described some of the horrific scenes that remain with him. Ongoing high stress, extra hours, and politicizing of healthcare can all add up to individuals who find themselves in a career crossroads that they don’t want to be in.
Though 44 healthcare systems were recently recognized by the AMA for their efforts to support clinicians’ well-being amid potential burnout, recent research shows that “burnout and a sense of hopelessness and compassion fatigue [are] escalating as this next COVID surge continues.”
Organizations have a big challenge to support their staff, restore a sense of normalcy, and provide mental health resources. Restoring balance seems to be in the details, with a campaign of interventions and changes that add up to a sustainable culture change. Such issues are not solved overnight; instead, consistent organizational responses to them can create an enormous difference.
For more on prioritizing mental health support of those in healthcare, click here.
Cybersecurity
Cybersecurity ranked the lowest in our survey, but many experts recommend it ranking as a higher priority. While we don’t yet have a comprehensive look at cybersecurity breaches of 2021, we do know that 2020 was the costliest year yet. The cost per ransomware breach came in at $4.62 million.
This trend doesn’t seem to be slowing down, and healthcare is the largest target. Healthcare spending on cybersecurity lags behind other areas such as finance, but the risk is higher. Prioritizing upgrades, conducting risk assessments, and maintaining ongoing security measures should rank high on healthcare leaders’ to-do lists going into the new year.

For more information on the latest in healthcare information technology and cybersecurity, click here.
Tackling upcoming healthcare challenges
Those in healthcare tend to focus on challenges, but it’s important to recognize and celebrate victories as well. The industry is coming out of a 2-year period of unprecedented change, arduous work, and resiliency. A recovery period is needed, a time to regroup and focus on lessons learned.
That period also calls for leaders to look ahead into 2022 and beyond and plan how they will tackle challenges ahead. Having the right mix of experts both on the front line and behind the scene is crucial to creating sustainable change.
From reimbursement to population health to health information technology, we’re here to support providers on a national basis and across all care settings. Our experts empower healthcare organization success, enhance clinical and financial outcomes, and enable the transition to value-based healthcare.
Kick-start your journey with us today:




