Addressing CDI Challenges: A Guide on How to Handle the Problem List

AHIMA indicates that problem lists should be standardized and designed to support an interdisciplinary and patient-centered approach for all provider health record entries. An up-to-date and accurate problem list is critical to the success of organizations providing patient care across the continuum of care in all settings.*
Well-designed problem lists provide important information for patient care and support meaningful use requirements and health information exchange. While there are many approaches to a well-designed problem list, the key is to define clear policies and procedures that support your organization’s objectives in using the information in a problem list.
Specifically, they need to address whether editing is permissible by roles other than independent licensed professionals who can make medical diagnoses. If so, those roles should be specified in the organization’s privileging policies and their responsibilities in terms of authorship should be clearly stated.
Your healthcare organization must ensure their policies and procedures for problem lists set standards that apply to their operational needs and future health information exchange uses with other providers. This is done while meeting the needs of the patient.
*Citation: AHIMA. “Definition, History, and Use of the Problem List.” Journal of AHIMA 90, no. 7 (Jul-Aug 2019)
The Primary Goals of a Policy for CDI Interacting Within the Problem List Include:
- Problem list accuracy
- Revenue protection of OIG/RADV targeted diagnoses
- Maximizing efficiencies in the future capture of EHR automated features for 2024 RAF capture of re-certified conditions
- Identify education opportunities
- Minimizing clutter
A Sample Policy Includes Both Diagnoses Additions and Deletions
Problem List Policy Additions Where the CDI Nurse Can Add Diagnoses If:
- Documentation is in the provider encounter note such as:
- Encounter HPI, A&P, PE (such as amputations)
- Status code of amputation, stomas, GT in PE, or ROS
- ICD-10 Guideline support such as:
- DM ‘with’ where both conditions in same DOS encounter note but not billed with a combination code
- Old MI (>4 weeks)
- BMI code
- Status codes (i.e., AKA, GT, etc.)
Some actual examples that were added in a case study as a result of the hospital policy:
- Dementia
- AAA
- CVA with hemiparesis
- DM2 with CKD, with neuropathy, with PVD, etc.
- CKD III, CKD IV
- Morbid obesity
- Skin ulcers
- History of breast, prostate cancer
- Secondary cancer
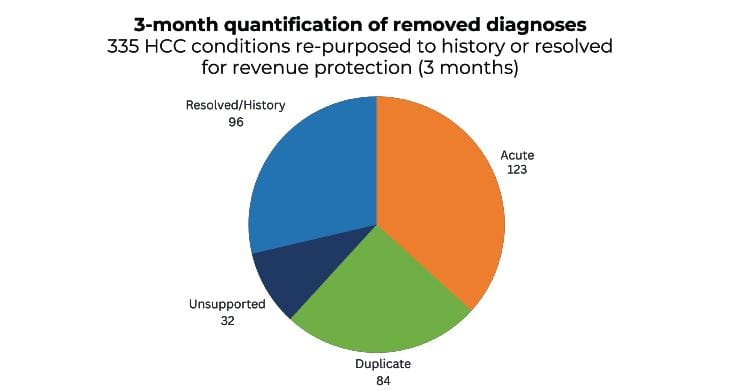
Problem List Policy Deletions Where the CDI Nurse Resolved or Deleted Diagnoses:
- Duplication
- Same diagnosis multiple times
- ICD-10 Guidelines:
- CVA acute event
- AMI occurrence over 4 weeks
- Documentation in the provider encounter note negating an active event:
- e., ‘history breast cancer s/p lumpectomy in 2008, Anastrozole completed 2013’
- Acute conditions resolved and added to history:
- Fractures
- Sepsis
- AKI
- PNA
- Unsupported diagnoses:
- Morbid obesity
- BMI
Some actual examples that were deleted or resolved in a case study as a result of the hospital policy:
- AMI, STEMI, NSTEMI
- CVA
- Unsupported
- Morbid obesity
- CKD III, IV, V
- Thrombocytopenia
- Resolved
- Cancer
- Skin
- PNA
- Sepsis
- AKI
- Acute respiratory failure
Conclusion
A policy that is developed and incorporated in the CDI role will support continuity of care with accurate up-to-date diagnoses supporting documentation integrity and revenue protection for your organization.
Addendum
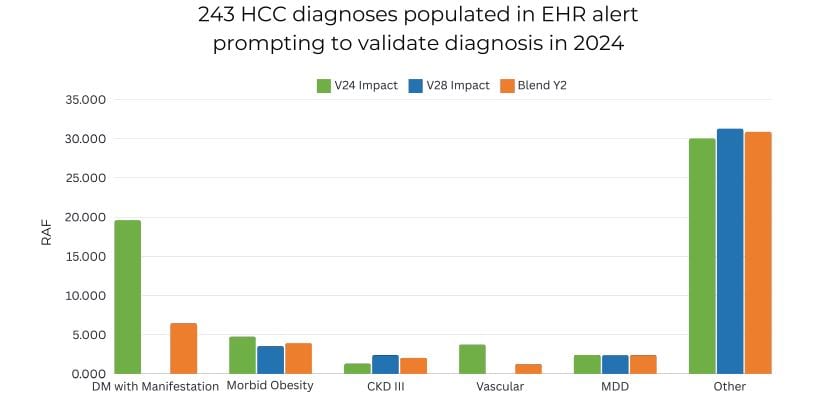
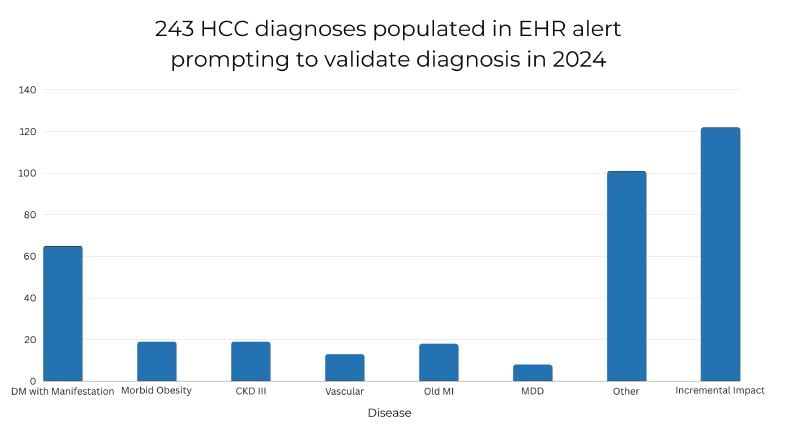
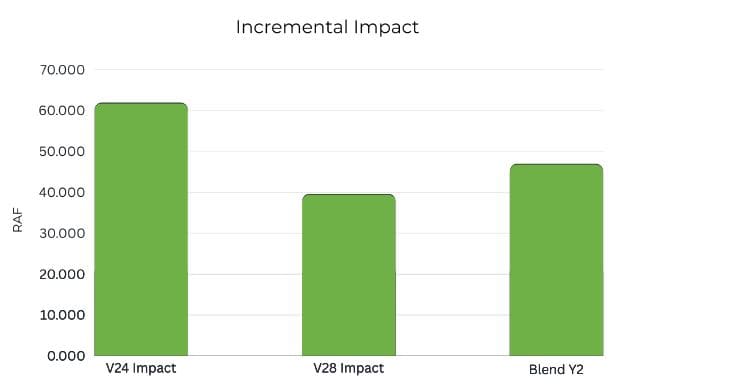
- 3 – Month Outcomes with 13 Providers
If you’re having trouble addressing CDI challenges or looking for your next CDI position, Harmony Healthcare is here to help. Contact us to learn more about how we can help you.





